Chronic wounds are those that do not progress through a normal, orderly, and timely sequence of repair.1 About 2 – 6% of the worldwide population require wound care for chronic wounds.2 Personal protective equipment, good waste management, comprehensive documentation, and management of the patient environment are all basic components of infection prevention in chronic wound care. A properly conducted dressing change, including an aseptic technique, is important to avoid cross contamination and spreading microbes between patients.3 The following instructions aim to protect your patients, their relatives, and yourself.
Appropriate wound management can contribute to better healing rates, fewer antibiotic prescriptions, improved quality of life and wellbeing for patients, and significant cost savings.4
Preparations [3]
Consider the following basic recommendations before each dressing change:
- Inform your patient about the upcoming dressing change.
- Use personal protective equipment such as a protective coat, face mask and eye protection, if needed.
- Disinfect a clean, flat, and non-porous work area for your equipment.
- Prepare all required equipment. Keep sterile material away from the patient, and place non-sterile material close to the patient.
- Avoid unnecessary interference, such as uninvolved people or pets. Close windows and doors to avoid cross contamination.
- Ensure that your patient is comfortable, the wound is easily accessible, and the lighting conditions are good.
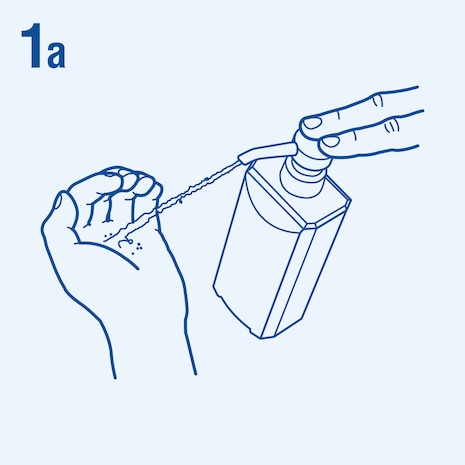
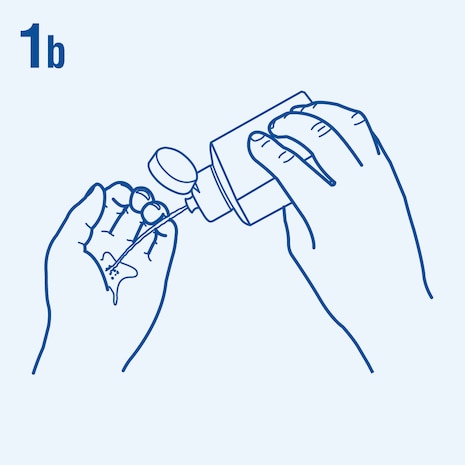
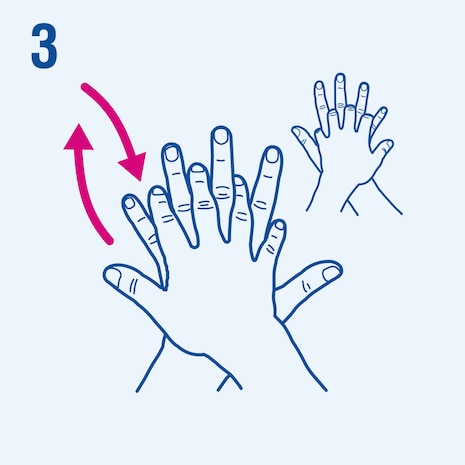
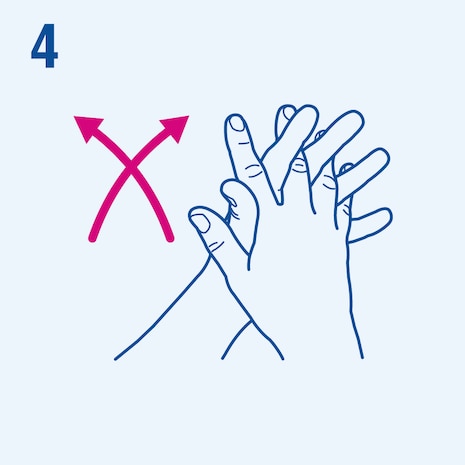
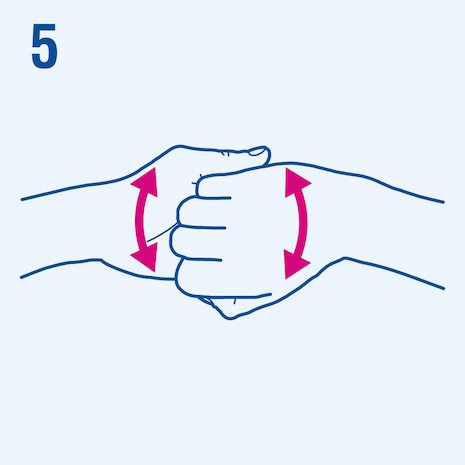
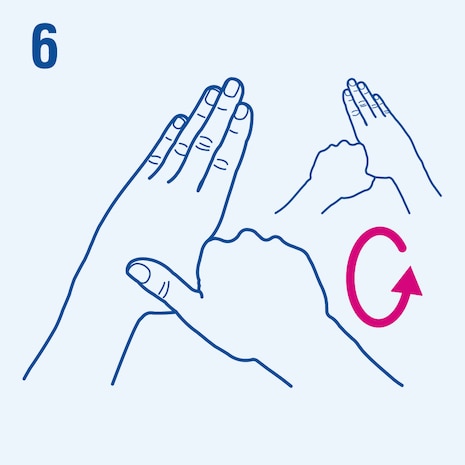
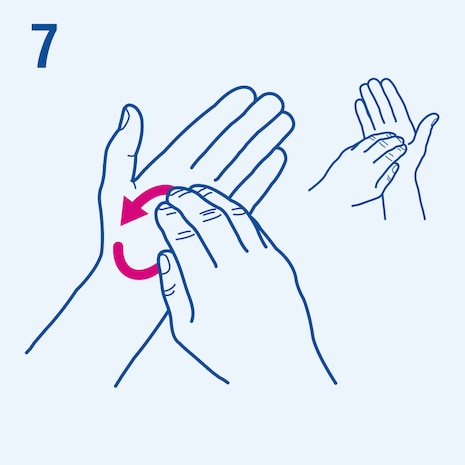
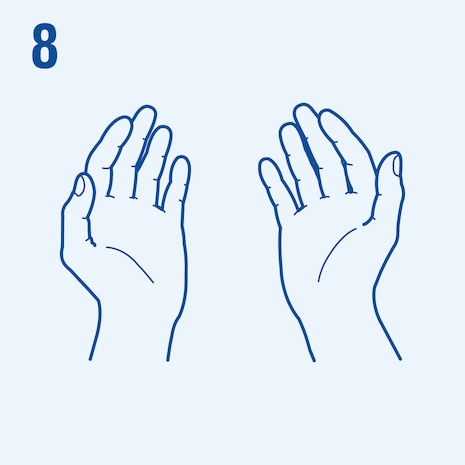
Consider the following steps when performing hand hygiene4. The duration of the entire procedure is 20-30 seconds.
| Clean / standard technique | Sterile / surgical technique | ||
| Smaller wound | Extensive wound | ||
| Simple and short dressing change (< 20 minutes) | Complex and longer dressing change (> 20 minutes) | ||
| Patient is not immuno-compromised | Patient is immuno-compromised | ||
| Palliative or maintenance care | Wound penetrates sterile body cavity or materials are inserted into a sinus or cavity where the wound base not visible | ||
| Clean your hand with alcohol-based sanitizer or skin cleanser and running water | Clean your hand with alcohol-based sanitizer or skin cleanser and running water | ||
| Wear non-sterile or sterile gloves | Wear sterile gloves | ||
| Use clean equipment, a basic dressing tray, and potable water (or sterile fluid) | Perform the dressing change in a sterile field with sterile equipment, including sterile cleansing solutions | ||
| Use clean or sterile, single-use wound dressing products | Use sterile, single-use wound dressing products |
Treat patients with non-infected wounds first before treating patients with infected wounds.
Complete the dressing change [3]
- Dispose infectious waste and sharps appropriately.
- Document the wound assessment (including color, odor, exudate, etc.), wound measurements and the procedures performed.
- Perform final hand hygiene.
Recognizing infected wounds
According to the wound infection continuum (framework to visualize the impact that microorganisms have on the host, the wound and on wound healing), a wound passes different conceptual stages until it is considered an infected wound3:
Microbial organisms are detectable but do not proliferate and do not evoke a host response.
Microbial organisms proliferate but do not evoke a significant host response.

Microbial organisms proliferate and evoke a host response and often includes a delay in wound healing.
- Excessive vascular tissue (hypergranulation)
- Bleeding, friable granulation
- Epithelial bridging and pocketing in granulation tissue
- Increasing exudate
- Delayed wound healing
- Superficial reddening (erythema)
- Local warmth
- Swelling
- Wound breakdown and enlargement
- New or increasing pain
- Increasing malodor
The above symptoms may be masked in people with compromised immune systems and/or poor vascular perfusion.
Infective organisms spread from the wound to the surrounding tissue. Signs of spreading infection are:
- Extending induration
- Spreading erythema
- Lymphangitis
- Crepitus
- Wound breakdown/dehiscence with or without satellite lesions
- Inflammation, swelling of lymph glands
Infective organisms spread via the lymphatic or vascular system and evoke a systemic reaction, resulting in sepsis and organ dysfunction. Systemic infection can lead to:
- Malaise
- Lethargy or nonspecific general deterioration
- Loss of appetite
- Fever
- Severe sepsis
- Septic shock
- Organ failure
- Death
Suspected spreading and systemic infections seek urgent medical attention. Usually, a swab will be taken according to medical recommendations and a suitable wound irrigation solution will be applied if needed. Antibiotic therapy is indicated and should be started immediately and adapted while waiting for the culture results.6
Continuous, accurate, holistic assessment of the individual and their wound is essential for effective wound treatment.3
Dressings with an antimicrobial effect can be used to support infection management. Consider wound dressings with Sorbact® Technology, such as Cutimed® Sorbact®6:
- Cutimed® Sorbact® binds, inhibits, and removes hydrophobic microbes with a purely physical mode of action. Cutimed® Sorbact® has no expected release of active substances into the wound.
- These dressings can be used for infection management on clean contaminated, colonized or infected wounds.
- Cutimed® Sorbact® is suitable for any kind of wound at all stages and can be used for a prolonged period of time.*
Disclaimer
*This article is intended to be used as an information guide to be considered when the organization makes clinical decisions and does not constitute medical advice. For detailed device information, including indications for use, contraindications, effects, precautions, and warnings, please consult the product’s Instructions for Use (IFU) before use. In case of doubt, please consult a healthcare professional.
References
- Bowers S & Franco E. Chronic Wounds: Evaluation and Management. Am Fam Physician. 2020; 101(3):159-166.
- Järbrink K, et al. The humanistic and economic burden of chronic wounds: a protocol for a systematic review. Syst Rev. 2017;6(1):15.
- International Wound Infection Institute (IWII) Wound infection in clinical practice. Wounds International. 2022.
- Murphy C, et al. International consensus document. Defying hard-to-heal wounds with an early antibiofilm intervention strategy: wound hygiene. J Wound Care. 2020; 29(Suppl 3b):S1–28.
- World Health Organization (WHO). Hand Hygiene Technical Reference Manual. WHO. 2009; accessed on November 4, 2022. Read more
- Best Practice Statement: Antimicrobial stewardship strategies for wound management. Wounds UK, London. 2020.